New "what if" scenarios by Mayo Clinic researchers show that Minnesota would be on the upswing of a devastating COVID-19 wave this spring if not for vaccine.
Factoring in more infectious variants of the SARS-CoV-2 virus and less mask-wearing and other protective measures, the researchers projected a peak of more than 800 COVID-19 patients needing hospital intensive care at once in Minnesota if nobody had been vaccinated. That more than doubles the actual record of 399 COVID-19 patients in Minnesota ICU beds on Dec. 1 at the height of the last pandemic wave.
"It is difficult to untangle how much of this elevated rate of spread right now is due to new variants as opposed to changes in social behavior," the authors wrote in a study released online Thursday before publication in the journal Mayo Clinic Proceedings. "Regardless of the reason, the absence of vaccinations in the current environment would have been likely to result in by far the largest surge to date."
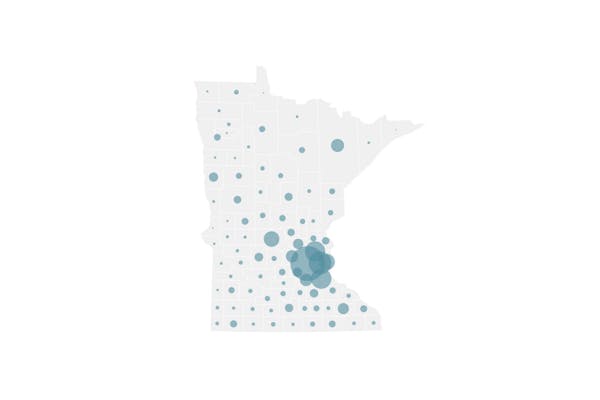
In reality, Minnesota has surged ahead of most states in its vaccination progress — providing at least first doses to nearly 2.2 million people or 50% of the eligible population 16 and older. And more than 84% of senior citizens have received vaccine — offering protection to a high-risk group that has suffered 89% of Minnesota's 6,995 COVID deaths.
Even so, health officials are concerned about the rising spread of the SARS-CoV-2 virus that causes COVID-19. The state on Friday reported six more COVID-19 deaths and 2,299 infections — raising the total case count to 552,117. The positivity rate of COVID-19 diagnostic testing also rose to 7.4% — above the state caution threshold of 5%.
COVID-19 hospitalizations in Minnesota had risen from a low of 210 on March 6 to 699 on Wednesday, but declined to 671 on Thursday. The latest total included 165 patients needing intensive care.
"We really, truly are in a race against time to get Minnesotans protected," state Health Commissioner Jan Malcolm said.
While a more infectious B.1.1.7 variant, first identified in England, is causing the majority of new infections in Minnesota, health officials on Friday urged people to avoid foreign travel to avoid spreading other variants.
Those who do travel should seek testing upon return and, if unvaccinated, quarantine themselves and monitor for symptoms.
Four Minnesotans from different households tested positive for the P.1 variant first identified in Brazil following travel to the Grand at Moon Palace in Cancun, Mexico, between March 12 and 23. Genomic sequencing of a small sampling of infections in Minnesota has found 20 related to P.1, which has shown potential for vaccine resistance.
A sign of hope in this latest wave is that COVID-19 deaths haven't increased over the past month at the same rate as infections and hospitalizations — possibly because so many high-risk people have been vaccinated. Hospital outcomes also have improved as the average age of admitted patients has dropped below 60.
State leaders want to reach an 80% vaccination rate among eligible Minnesotans to achieve a level of herd immunity that would stifle viral spread. Gov. Tim Walz on Friday made an appeal specifically to manufacturing workers to sign up for vaccination slots on the Minnesota Vaccine Connector (vaccineconnector.mn.gov/en-US/) because of their elevated workplace risks of viral exposure.
"They have worked so hard during this unprecedented crisis to keep everything from food on our tables to PPE on our shelves, and now we're going to make sure each and every one of them gets easy and convenient access to vaccines," Walz said.
Minneapolis-based Allina Health also expanded vaccine access on Friday, offering shots to any of its patients 50 or older.
The Mayo study was led by Curtis Storlie and Dr. Sean Dowdy, who developed a model for forecasting COVID-19's impact on hospital usage. It also found that continued vaccination is necessary.
Had all vaccination activity ceased on April 6, the most likely scenario under the modeling is that Minnesota would have come close to 300 COVID-19 ICU admissions. Had Minnesota magically reached a 75% vaccination rate on that date, the modeling suggested that viral activity and hospital usage would have quickly dissipated.
The Mayo projections carry the same uncertainties as the many U.S. models predicting pandemic activity — with changes in public behaviors and the emergence of viral variants challenging the assumptions on which their results are based.
Storlie said the results of the Mayo research urge continued vaccination, showing that the current wave could be lengthened in the absence of more people receiving shots.
"To me that is the big difference," he said in an e-mail, "not how high [the wave] would get, but how much longer we all have to deal with it — i.e., let's put an end to this nightmare sooner."
Jeremy Olson • 612-673-7744

Icehouse owner hopes to avoid evection as music scene rallies around Eat Street venue
Edina man admits to fatally shooting a man in Minneapolis during dispute over money

After an ATF ruling, the bottom falls out for a St. Cloud firearms manufacturer

Duluth mayor pledges population growth in the long-stalled city